Author: Veronica Varela
Editors: Whit Froehlich, John Charpentier, and Scott Barolo
Cervical cancer has been getting much more attention as of late, partly due to the HBO adaptation of Rebecca Skloot’s book The Immortal life of Henrietta Lacks. As a survivor of the same type of cancer that took Henrietta’s life and led to the development of the HeLa cell line, I found that Skloot’s book resonated deeply with me. My diagnosis compelled me to learn more about cervical cancer, which is one of the most preventable forms of cancer.
What Is Cervical Cancer?

Cervical cancer is an abnormal and uncontrolled growth of the cells lining the cervix, which acts like the doorway to the uterus. The cervix lining is mostly made up of two different cell types. Lining the outer cervix that faces the vagina are squamous cells, which are flat in shape, while the open passage of the cervix which leads into the uterus is lined by glandular cells, which are blockier in shape and produce mucus. Cancer can arise from either of these cell types; however, squamous cell cancers are the more frequent.
Most cervical cancers are caused by Human Papilloma Virus (HPV). HPV is commonly known as the virus that causes genital warts, but what many don’t realize is that there are over a dozen types of sexually transmitted HPVs, and only a few of them result in genital warts. The National Institutes of Health (NIH) highlight that persistent infection with certain HPV strains, especially types 16 and 18, is the major cause of most cervical cancer cases.

For many, an HPV infection carries a stigma, something only “promiscuous” people worry about. In truth, HPV infections are incredibly common in the United States; the CDC reports that most sexually active men and women will be infected with a type of HPV at some point in their lifetime.
Because of the high prevalence and connection to cervical cancer, HPV infection is a significant public health issue. Vaccines are available for HPV types 6, 9, 11, 16, 18, 31, 33, 45, 52, and 58. The vaccines are virus-like particles, not actual viruses that can cause infections. However, for those who are already sexually active, these vaccines are not as effective. Cervical cancer screening is available through Pap smears, which are recommended every three years for women between the ages of 21 and 65.
While cervical cancer is typically thought of as slow-progressing cancer, each cancer is different and some may progress more quickly. My own case was a fast-developing cancer: I went from one negative Pap smear to carcinoma in situ when I was next screened, for which I ultimately underwent a radical hysterectomy. Being consistent with screenings is important to catching this treatable cancer early.
The standard treatments for early-stage cervical cancers range from removing only the lesion to complete hysterectomy. But later-stage cancers that have spread to other organs are more difficult to treat. Identifying effective treatments for later-stage cancers has been a major challenge in cancer research.
Recent Advances in Cervical Cancer Treatments
Immunotherapies are becoming a popular form of cancer treatment. Antibodies can now be created on a large scale and tailored to attack cancer-specific targets. Much of cancer treatment research goes into finding these cancer-specific targets, allowing drugs to spare normal tissue. Effective targeted therapies have been developed, but they are limited to a few types of cancers; for example, some breast cancers overexpress HER-2, a receptor that promotes cellular survival and proliferation. The increased levels of HER-2 make it a viable treatment target, and a HER2-targeting antibody has been developed that treats many breast cancers.
More recently, other targets with the potential to treat a broader scope of cancers have been discovered. Among these are immune system checkpoint proteins, which effectively tell immune cells to stand down. Cancer cells often use these same signals to avoid being attacked by the immune system. With therapies targeting immune checkpoints, the immune system can be jump-started back up to fight against cancers. Many of these are in clinical trials, with promising results, although much research remains to be done to identify side effects, since they work throughout the whole body, not just at the tumor. Other types of therapies include oncolytic viruses, which are designed to more easily infect cancer cells, recruiting immune cells to the site of infection while sparing normal cells.
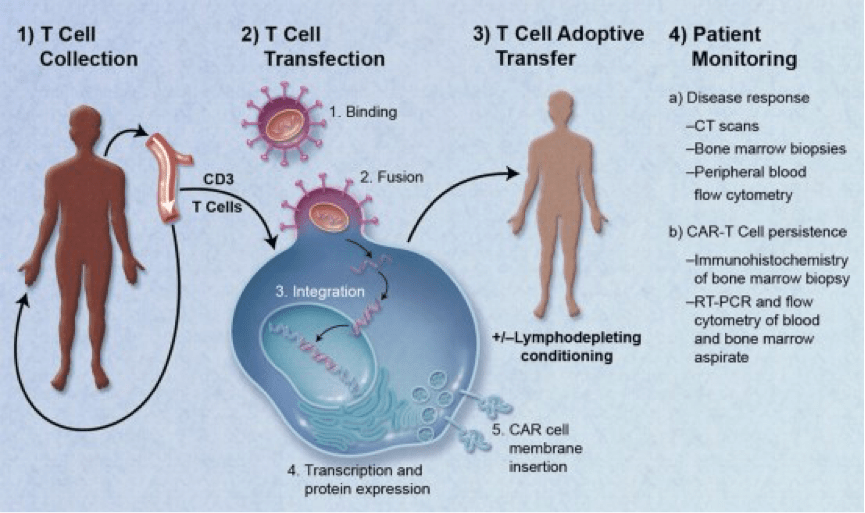
Chimeric antigen receptor T-cell (CAR-T) therapy is another new immunotherapy. With CAR-T therapy, immune cells are reprogrammed to attack cancer cells. T-cells are the main killer cells of the immune system and, like antibodies, each has a specific target it can recognize. Many cancers aren’t recognized by these killer cells. T-cells can be isolated from a patient’s blood and programmed to recognize and attack only cancer cells. These reprogrammed cells are multiplied and then infused back into the patient, where they go to work to attack cancer. Researchers are encouraged by the results of this treatment so far, with many studies in the clinical trial stage; and one CAR-T therapy was recently recommended for approval by the FDA for treatment of B-cell acute lymphoblastic leukemia.
Interleukin-2 (IL-2), a protein made by some immune cells, is another treatment being studied to combat cancer. IL-2 causes T-cells to multiply, among other things, leading to increased immune responses. Each of these therapies has drawbacks, and more research is required to refine the best techniques.
Not all therapies utilize the immune system, as many cellular growth signals make promising treatment targets. These targeted therapies involve using selective drugs, rather than antibodies, to either stop the signals cancer uses to grow or tell the cancer to kill itself. Researchers are increasing their knowledge about the genetic changes that occur in tumor cells and using this information can develop drugs specifically targeting the gene products that that drive them. Such therapies are usually used in combination with chemotherapy drugs, as they can also make traditional chemotherapies more effective.
Some techniques help make current treatments more effective and efficient, such as Sentinel Lymph Node Biopsy (SLNB), a procedure used during surgery. It is common practice to remove the lymph nodes in the pelvis to screen for metastasis of cervical cancer but through SNLB doctors can identify lymph nodes that contain cancer. A dye tracer is injected into the area around the main tumor, and will travel to the nearest lymph nodes, which is where metastatic cancer is also most likely to go. Lymph nodes containing the tracer can then be removed and screened for signs of cancer, letting doctors know whether it has spread or not. Clinical trials are investigating the combination of SNLB with laproscopic surgery for less invasive procedures. Research suggests SNLB is more effective in early stage cervical cancers.
Disparities in Cervical Cancer Screening and Treatment
These developments in treating even metastatic cancer are encouraging, but unfortunately few women actually receive screening and treatment. A recent study found that cervical cancer death rates were significantly higher than had been previously reported in the United States, which is a shame since it is one of the most preventable cancers. This study corrected previously published data by excluding women who had undergone hysterectomies, making them unable to develop cervical cancer. In the original studies, the data used to calculate mortality rates included women who received hysterectomies and thus had no cervix, which led to an understatement of the risk.
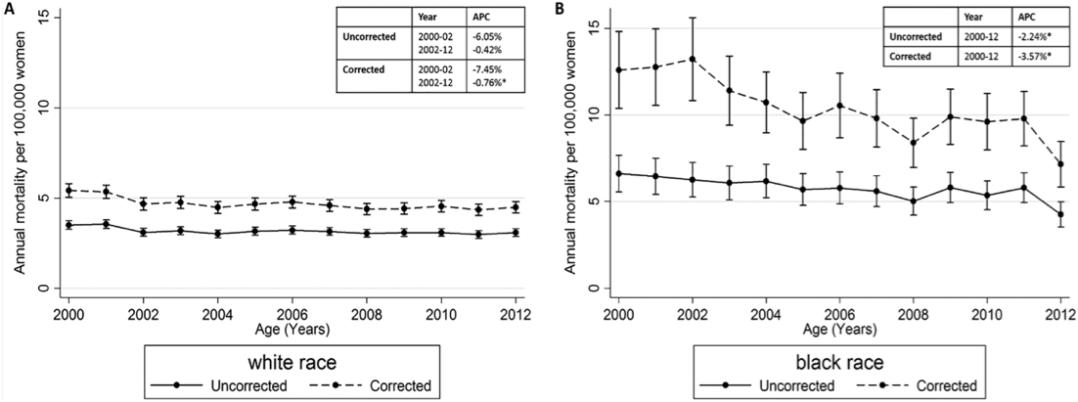
However, this study is still not a complete picture of the true disparity in incidence and mortality rates of cervical cancer between women of color and white women, since it excludes other significant minority populations, such as Hispanic/Latina women. The NIH National Cancer Institute (NCI) website’s statistics for 2000-2004 show that Hispanic/Latina women have the highest incidence of cervical cancer, whereas African American/Black women have the highest death rates. This disparity is due to unequal access to health care and a lack of screening in these populations. There is a significant association between lower socioeconomic status and incidence/mortality. The easier it is to access healthcare, the more frequent screening will be and the likelihood of diagnosing cervical cancer at an early stage is increased.
“Nowhere is this failure of our health care system more apparent than in the disparities in cervical cancer incidence and outcome… suffered by members of particular racial and ethnic minority subgroups and other underserved populations… Cervical cancer (is) a disease for which effective prevention—not just early detection—and treatment have existed for decades.” – Harold P. Freeman, M.D., National Cancer Institute
Incidence and death rates in Texas alone are twice as high as the national average, according to the NIH. 18% of the Texan population remain without health insurance and many of those that do still can’t afford routine screenings because their deductibles are too high. The South, in general, has increased mortality rates compared to the national average. A recent study outlined the age-specific differences seen in incidence and mortality between Southern non-Hispanic whites (NHW) and non-Hispanic blacks (NHB), showing that NHB women have a significantly higher incidence and mortality at all ages.

Given this data, expanding affordable access to screening services would help address this disparity, but these initiatives must be targeted to at-risk populations and practitioners need to be made aware of these issues to help tackle the problem.
Follow the links below for more information on cervical cancer:
Find out more about ways to reduce cervical cancer mortality in vulnerable populations
NIH/NCI Division of Cancer Control & Population Sciences
Cervical Cancer Health Disparities Fact Sheet
*An earlier version of this post was published here.
About the author:

Veronica Varela is currently 5th-year Ph.D. student in Neuroscience at the University of Michigan. After taking eight years off of school, Veronica balanced lab work, classes, homework and raising two daughters, while earning her bachelor’s degree in psychology from California State University, San Bernardino. She is currently investigating the role the molecular circadian clock plays in regulating sleep timing. As a mom and cancer survivor, Veronica knows how life’s challenges can impede educational goals and is committed to improving diversity, inclusion, and equal opportunity in STEM fields which led to her creating Science in Color with her husband and a group of colleagues, an organization focused on increasing representation, visibility, recruitment, and retention of marginalized groups. Follow her on Twitter or LinkedIn.
Read all posts by Veronica here.
Image credits:
Figure 1: upload.wikimedia.org/wikipedia/commons/thumb/b/bd/Diagram_showing_stage_4A_cervical_cancer_CRUK_236.svg/703px-Diagram_showing_stage_4A_cervical_cancer_CRUK_236.svg.png
Figure 2: upload.wikimedia.org/wikipedia/commons/7/7c/Papilloma_virus_%28hpv%29.jpg
Figure 3: upload.wikimedia.org/wikipedia/commons/a/a2/CAR-Engineered_T-Cell_Adoptive_Transfer.jpg
Figure 4: http://onlinelibrary.wiley.com/doi/10.1002/cncr.30507/full
Figure 5: http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0172548

Each year, about 13,000 cases of cervical cancer are diagnosed in the United States. There are approximately 4,000 deaths per year due to cervical cancer.
https://everydayscience.blog/cervical-cancer-symptoms-signs/
LikeLike